SARS facts for kids
Quick facts for kids Severe acute respiratory syndrome(SARS) |
|
|---|---|
| Synonyms | Sudden acute respiratory syndrome |
 |
|
| Electron micrograph of SARS coronavirus virion | |
| Pronunciation | |
| Symptoms | Fever, persistent dry cough, headache, muscle pains, difficulty breathing |
| Complications | Acute respiratory distress syndrome (ARDS) with other comorbidities that eventually leads to death |
| Duration | 2002–2004 |
| Causes | Severe acute respiratory syndrome coronavirus (SARS-CoV-1) |
| Prevention | N95 or FFP2 respirators, ventilation, UVGI, avoiding travel to affected areas |
| Prognosis | 9.5% chance of death (all countries) |
| Frequency | 8,096 cases total |
| Deaths | 783 known |
Severe acute respiratory syndrome (SARS) is a viral respiratory disease of zoonotic origin caused by the virus SARS-CoV-1, the first identified strain of the SARS-related coronavirus. The first known cases occurred in November 2002, and the syndrome caused the 2002–2004 SARS outbreak. In the 2010s, Chinese scientists traced the virus through the intermediary of Asian palm civets to cave-dwelling horseshoe bats in Xiyang Yi Ethnic Township, Yunnan.
SARS was a relatively rare disease; at the end of the epidemic in June 2003, the incidence was 8,469 cases with a case fatality rate (CFR) of 11%. No cases of SARS-CoV-1 have been reported worldwide since 2004.
In December 2019, a second strain of SARS-CoV was identified: SARS-CoV-2. This strain causes coronavirus disease 2019 (COVID-19), the disease behind the COVID-19 pandemic.
Contents
Signs and symptoms
SARS produces flu-like symptoms which may include fever, muscle pain, lethargy, cough, sore throat, and other nonspecific symptoms. The only symptom common to all patients appears to be a fever above 38 °C (100 °F). SARS often leads to shortness of breath and pneumonia, which may be direct viral pneumonia or secondary bacterial pneumonia.
The average incubation period for SARS is 4–6 days, although it is rarely as short as 1 day or as long as 14 days.
Transmission
The primary route of transmission for SARS-CoV is contact of the mucous membranes with respiratory droplets or fomites. As with all respiratory pathogens once presumed to transmit via respiratory droplets, it is highly likely to be carried by the aerosols generated during routine breathing, talking, and even singing. While diarrhea is common in people with SARS, the fecal–oral route does not appear to be a common mode of transmission. The basic reproduction number of SARS-CoV, R0, ranges from 2 to 4 depending on different analyses. Control measures introduced in April 2003 reduced the R to 0.4.
Diagnosis
SARS-CoV may be suspected in a patient who has:
- Any of the symptoms, including a fever of 38 °C (100 °F) or higher, and
- Either a history of:
- Contact with someone with a diagnosis of SARS within the last 10 days or
- Travel to any of the regions identified by the World Health Organization (WHO) as areas with recent local transmission of SARS.
- Clinical criteria of Sars-CoV diagnosis
- Early illness: equal to or more than 2 of the following: chills, rigors, myalgia, diarrhea, sore throat (self-reported or observed)
- Mild-to-moderate illness: temperature of >38 °C (100 °F) plus indications of lower respiratory tract infection (cough, dyspnea)
- Severe illness: ≥1 of radiographic evidence, presence of ARDS, autopsy findings in late patients.
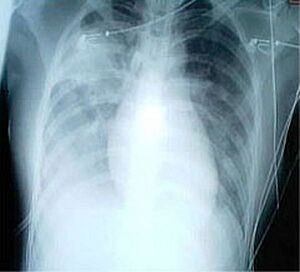
For a case to be considered probable, a chest X-ray must be indicative for atypical pneumonia or acute respiratory distress syndrome.
The WHO has added the category of "laboratory confirmed SARS" which means patients who would otherwise be considered "probable" and have tested positive for SARS based on one of the approved tests (ELISA, immunofluorescence or PCR) but whose chest X-ray findings do not show SARS-CoV infection (e.g. ground glass opacities, patchy consolidations unilateral).
The appearance of SARS-CoV in chest X-rays is not always uniform but generally appears as an abnormality with patchy infiltrates.
Prevention
There is a vaccine for SARS, although in March 2020 immunologist Anthony Fauci said the CDC developed one and placed it in the Strategic National Stockpile. That vaccine is a final product and field-ready as of March 2022. Clinical isolation and vaccination remain the most effective means to prevent the spread of SARS. Other preventive measures include:
- Hand-washing with soap and water, or use of alcohol-based hand sanitizer
- Disinfection of surfaces of fomites to remove viruses
- Avoiding contact with bodily fluids
- Washing the personal items of someone with SARS in hot, soapy water (eating utensils, dishes, bedding, etc.)
- Avoiding travel to affected areas
- Wearing masks and gloves
- Keeping people with symptoms home from school
- Simple hygiene measures
- Distancing oneself at least 6 feet if possible to minimize the chances of transmission of the virus
Many public health interventions were made to try to control the spread of the disease, which is mainly spread through respiratory droplets in the air, either inhaled or deposited on surfaces and subsequently transferred to a body's mucous membranes. These interventions included earlier detection of the disease; isolation of people who are infected; droplet and contact precautions; and the use of personal protective equipment (PPE), including masks and isolation gowns. A 2017 meta-analysis found that for medical professionals wearing N-95 masks could reduce the chances of getting sick up to 80% compared to no mask. A screening process was also put in place at airports to monitor air travel to and from affected countries.
SARS-CoV is most infectious in severely ill patients, which usually occurs during the second week of illness. This delayed infectious period meant that quarantine was highly effective; people who were isolated before day five of their illness rarely transmitted the disease to others.
As of 2017, the CDC was still working to make federal and local rapid-response guidelines and recommendations in the event of a reappearance of the virus.
Treatment
As SARS is a viral disease, antibiotics do not have direct effect but may be used against bacterial secondary infection. Treatment of SARS is mainly supportive with antipyretics, supplemental oxygen and mechanical ventilation as needed. While ribavirin is commonly used to treat SARS, there seems to have little to no effect on SARS-CoV, and no impact on patient's outcomes. There is currently no proven antiviral therapy. Tested substances, include ribavirin, lopinavir, ritonavir, type I interferon, that have thus far shown no conclusive contribution to the disease's course. Administration of corticosteroids, is recommended by the British Thoracic Society/British Infection Society/Health Protection Agency in patients with severe disease and O2 saturation of <90%.
People with SARS-CoV must be isolated, preferably in negative-pressure rooms, with complete barrier nursing precautions taken for any necessary contact with these patients, to limit the chances of medical personnel becoming infected. In certain cases, natural ventilation by opening doors and windows is documented to help decreasing indoor concentration of virus particles.
Some of the more serious damage caused by SARS may be due to the body's own immune system reacting in what is known as cytokine storm.
Vaccine
Vaccines can help the immune system to create enough antibodies and decrease a risk of side effects like arm pain, fever, and headache. According to research papers published in 2005 and 2006, the identification and development of novel vaccines and medicines to treat SARS was a priority for governments and public health agencies around the world. In early 2004, an early clinical trial on volunteers was planned. A major researcher's 2016 request, however, demonstrated that no field-ready SARS vaccine had been completed because likely market-driven priorities had ended funding.
Prognosis
Several consequent reports from China on some recovered SARS patients showed severe long-time sequelae. The most typical diseases include, among other things, pulmonary fibrosis, osteoporosis, and femoral necrosis, which have led in some cases to the complete loss of working ability or even self-care ability of people who have recovered from SARS. As a result of quarantine procedures, some of the post-SARS patients have been diagnosed with post-traumatic stress disorder (PTSD) and major depressive disorder.
Epidemiology
SARS was a relatively rare disease; at the end of the epidemic in June 2003, the incidence was 8,422 cases with a case fatality rate (CFR) of 11%.
The case fatality rate (CFR) ranges from 0% to 50% depending on the age group of the patient. Patients under 24 were least likely to die (less than 1%); those 65 and older were most likely to die (over 55%).
As with MERS and COVID-19, SARS resulted in significantly more deaths of males than females.
| Country or region | Cases | Deaths | Fatality (%) | |
|---|---|---|---|---|
| 5,327 | 349 | 6.6 | ||
| 1,755 | 299 | 17.0 | ||
| 346 | 81 | 23.4 | ||
| 251 | 43 | 17.1 | ||
| 238 | 33 | 13.9 | ||
| 63 | 5 | 7.9 | ||
| 27 | 0 | 0 | ||
| 14 | 2 | 14.3 | ||
| 9 | 2 | 22.2 | ||
| 9 | 0 | 0 | ||
| 9 | 0 | 0 | ||
| 7 | 1 | 14.3 | ||
| 6 | 0 | 0 | ||
| 5 | 2 | 40.0 | ||
| 5 | 0 | 0 | ||
| 4 | 0 | 0 | ||
| 4 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 1 | 1 | 100.0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| Total excluding China | 2,769 | 454 | 16.4 | |
| Total (29 territories) | 8,096 | 782 | 9.6 | |
Outbreak in South China
The SARS epidemic began in the Guangdong province of China in November 2002. The earliest case developed symptoms on 16 November 2002. The index patient, a farmer from Shunde, Foshan, Guangdong, was treated in the First People's Hospital of Foshan. The patient died soon after, and no definite diagnosis was made on his cause of death. Despite taking some action to control it, Chinese government officials did not inform the World Health Organization of the outbreak until February 2003. This lack of openness caused delays in efforts to control the epidemic, resulting in criticism of the People's Republic of China from the international community. China officially apologized for early slowness in dealing with the SARS epidemic. In 2003, when the virus broke out in China, a 72 year old with SARS infected multiple people on board an Air China Boeing 737, causing 5 deaths. The viral outbreak was subsequently genetically traced to a colony of cave-dwelling horseshoe bats in Xiyang Yi Ethnic Township, Yunnan.
The outbreak first came to the attention of the international medical community on 27 November 2002, when Canada's Global Public Health Intelligence Network (GPHIN), an electronic warning system that is part of the World Health Organization's Global Outbreak Alert and Response Network (GOARN), picked up reports of a "flu outbreak" in China through Internet media monitoring and analysis and sent them to the WHO. While GPHIN's capability had recently been upgraded to enable Arabic, Chinese, English, French, Russian, and Spanish translation, the system was limited to English or French in presenting this information. Thus, while the first reports of an unusual outbreak were in Chinese, an English report was not generated until 21 January 2003. The first super-spreader was admitted to the Sun Yat-sen Memorial Hospital in Guangzhou on 31 January, which soon spread the disease to nearby hospitals.
In early April 2003, after a prominent physician, Jiang Yanyong, pushed to report the danger to China, there appeared to be a change in official policy when SARS began to receive a much greater prominence in the official media. Some have directly attributed this to the death of an American teacher, James Earl Salisbury, in Hong Kong. It was around this same time that Jiang Yanyong made accusations regarding the undercounting of cases in Beijing military hospitals. After intense pressure, Chinese officials allowed international officials to investigate the situation there. This revealed problems plaguing the aging mainland Chinese healthcare system, including increasing decentralization, red tape, and inadequate communication.
Many healthcare workers in the affected nations risked their lives and died by treating patients, and trying to contain the infection before ways to prevent infection were known.
Spread to other regions
The epidemic reached the public spotlight in February 2003, when an American businessman traveling from China, Johnny Chen, became affected by pneumonia-like symptoms while on a flight to Singapore. The plane stopped in Hanoi, Vietnam, where the patient died in Hanoi French Hospital. Several of the medical staff who treated him soon developed the same disease despite basic hospital procedures. Italian doctor Carlo Urbani identified the threat and communicated it to WHO and the Vietnamese government; he later died from the disease.
The severity of the symptoms and the infection among hospital staff alarmed global health authorities, who were fearful of another emergent pneumonia epidemic. On 12 March 2003, the WHO issued a global alert, followed by a health alert by the United States Centers for Disease Control and Prevention (CDC). Local transmission of SARS took place in Toronto, Ottawa, San Francisco, Ulaanbaatar, Manila, Singapore, Taiwan, Hanoi and Hong Kong whereas within China it spread to Guangdong, Jilin, Hebei, Hubei, Shaanxi, Jiangsu, Shanxi, Tianjin, and Inner Mongolia.
Containment
The World Health Organization declared severe acute respiratory syndrome contained on 5 July 2003. The containment was achieved through successful public health measures. In the following months, four SARS cases were reported in China between December 2003 and January 2004.
While SARS-CoV-1 probably persists as a potential zoonotic threat in its original animal reservoir, human-to-human transmission of this virus may be considered eradicated because no human case has been documented since four minor, brief, subsequent outbreaks in 2004.
Laboratory accidents
After containment, there were four laboratory accidents that resulted in infections.
- One postdoctoral student at the National University of Singapore in Singapore in August 2003
- A 44-year-old senior scientist at the National Defense University in Taipei in December 2003. He was confirmed to have the SARS virus after working on a SARS study in Taiwan's only BSL-4 lab. The Taiwan CDC later stated the infection occurred due to laboratory misconduct.
- Two researchers at the Chinese Institute of Virology in Beijing, China around April 2004, who spread it to around six other people. The two researchers contracted it 2 weeks apart.
Study of live SARS specimens requires a biosafety level 3 (BSL-3) facility; some studies of inactivated SARS specimens can be done at biosafety level 2 facilities.
Society and culture
Fear of contracting the virus from consuming infected wild animals resulted in public bans and reduced business for meat markets in southern China and Hong Kong. The WHO declared the end of the pandemic on March 24 2004.
See also
- 2009 swine flu pandemic
- Aerosol
- Avian influenza
- Bat-borne virus
- Coronavirus disease 2019 – a disease caused by Severe acute respiratory syndrome coronavirus 2
- Health crisis
- Health in China
- Healthy building
- Indoor air quality
- List of medical professionals who died during the SARS outbreak
- Middle East respiratory syndrome – a coronavirus discovered in June 2012 in Saudi Arabia
- SARS conspiracy theory
- Sick building syndrome
- Zhong Nanshan



