Insomnia facts for kids
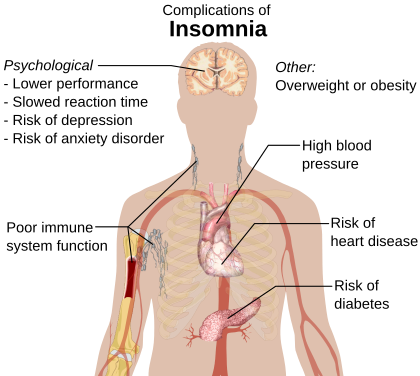
Quick facts for kids Insomnia |
|
|---|---|
| Synonyms | Sleeplessness, trouble sleeping |
 |
|
| Depiction of insomnia from the 14th century medical manuscript Tacuinum Sanitatis | |
| Symptoms | Trouble sleeping, daytime sleepiness, low energy, irritability, depressed mood |
| Complications | Motor vehicle collisions |
| Causes | Unknown, psychological stress, chronic pain, heart failure, hyperthyroidism, heartburn, restless leg syndrome, others |
| Diagnostic method | Based on symptoms, sleep study |
| Similar conditions | Delayed sleep phase disorder, restless leg syndrome, sleep apnea, psychiatric disorder |
| Treatment | Sleep hygiene, cognitive behavioral therapy, sleeping pills |
| Frequency | ~20% |
Insomnia, also known as sleeplessness, is a sleep disorder where people have trouble sleeping. They may have difficulty falling asleep, or staying asleep for as long as desired. Insomnia is typically followed by daytime sleepiness, low energy, irritability, and a depressed mood. It may result in an increased risk of motor vehicle collisions, as well as problems focusing and learning. Insomnia can be short term, lasting for days or weeks, or long term, lasting more than a month. The concept of the word insomnia has two possibilities: insomnia disorder and insomnia symptoms, and many abstracts of randomized controlled trials and systematic reviews often underreport on which of these two possibilities the word insomnia refers to.
Insomnia can occur independently or as a result of another problem. Conditions that can result in insomnia include psychological stress, chronic pain, heart failure, hyperthyroidism, heartburn, restless leg syndrome, menopause, certain medications, caffeine, nicotine, etc. Other risk factors include working night shifts and sleep apnea. Diagnosis is based on sleep habits and an examination to look for underlying causes. A sleep study may be done to look for underlying sleep disorders. Screening may be done with two questions: "do you experience difficulty sleeping?" and "do you have difficulty falling or staying asleep?"
Although their efficacy as first line treatments is not unequivocally established, sleep hygiene and lifestyle changes are typically the first treatment for insomnia. Sleep hygiene includes a consistent bedtime, a quiet and dark room, exposure to sunlight during the day and regular exercise. Cognitive behavioral therapy may be added to this. While sleeping pills may help, they are not recommended for more than four or five weeks. The effectiveness and safety of alternative medicine is unclear.
Between 10% and 30% of adults have insomnia at any given point in time and up to half of people have insomnia in a given year. About 6% of people have insomnia that is not due to another problem and lasts for more than a month. People over the age of 65 are affected more often than younger people. Women are more often affected than males. Descriptions of insomnia occur at least as far back as ancient Greece.
Signs and symptoms
Symptoms of insomnia:
- Difficulty falling asleep, including difficulty finding a comfortable sleeping position
- Waking during the night, being unable to return to sleep and waking up early
- Not able to focus on daily tasks, difficulty in remembering
- Daytime sleepiness, irritability, depression or anxiety
- Feeling tired or having low energy during the day
- Trouble concentrating
- Being irritable, acting aggressive or impulsive
Sleep onset insomnia is difficulty falling asleep at the beginning of the night, often a symptom of anxiety disorders. Delayed sleep phase disorder can be misdiagnosed as insomnia, as sleep onset is delayed to much later than normal while awakening spills over into daylight hours.
It is common for patients who have difficulty falling asleep to also have nocturnal awakenings with difficulty returning to sleep. Two-thirds of these patients wake up in the middle of the night, with more than half having trouble falling back to sleep after a middle-of-the-night awakening.
Early morning awakening is an awakening occurring earlier (more than 30 minutes) than desired with an inability to go back to sleep, and before total sleep time reaches 6.5 hours. Early morning awakening is often a characteristic of depression. Anxiety symptoms may well lead to insomnia. Some of these symptoms include tension, compulsive worrying about the future, feeling overstimulated, and overanalyzing past events.
Causes
While insomnia can be caused by a number of conditions, it can also occur without any identifiable cause. This is known as Primary Insomnia. Primary Insomnia may also have an initial identifiable cause, but continues after the cause is no longer present. For example, a bout of insomnia may be triggered by a stressful work or life event. However the condition may continue after the stressful event has been resolved. In such cases, the insomnia is usually perpetuated by the anxiety or fear caused by the sleeplessness itself, rather than any external factors.
Symptoms of insomnia can be caused by or be associated with:
- Sleep breathing disorders, such as sleep apnea or upper airway resistance syndrome
- Use of psychoactive stimulants, including certain medications, herbs, caffeine, nicotine, etc.
- Heart disease
- Restless legs syndrome, which can cause sleep onset insomnia due to the discomforting sensations felt and the need to move the legs or other body parts to relieve these sensations
- Periodic limb movement disorder (PLMD), which occurs during sleep and can cause arousals of which the sleeper is unaware
- Pain: an injury or condition that causes pain can preclude an individual from finding a comfortable position in which to fall asleep, and can also cause awakening.
- Hormone shifts such as those that precede menstruation and those during menopause
- Life events such as fear, stress, anxiety, emotional or mental tension, work problems, financial stress, birth of a child, and bereavement
- Gastrointestinal issues such as heartburn or constipation
- Mental, neurobehavioral, or neurodevelopmental disorders such as bipolar disorder, clinical depression, generalized anxiety disorder, post traumatic stress disorder, schizophrenia, obsessive compulsive disorder, autism, dementia, ADHD, etc.
- Disturbances of the circadian rhythm, such as shift work and jet lag, can cause an inability to sleep at some times of the day and excessive sleepiness at other times of the day. Chronic circadian rhythm disorders are characterized by similar symptoms.
- Certain neurological disorders such as brain lesions, or a history of traumatic brain injury
- Medical conditions such as hyperthyroidism
- Abuse of over-the-counter or prescription sleep aids (sedative or depressant drugs) can produce rebound insomnia
- Poor sleep hygiene, e.g., noise or over-consumption of caffeine
- A rare genetic condition can cause a prion-based, permanent and eventually fatal form of insomnia called fatal familial insomnia
- Physical exercise: exercise-induced insomnia is common in athletes in the form of prolonged sleep onset latency
- Increased exposure to the blue light from artificial sources, such as phones or computers
- Chronic pain
- Lower back pain
- Asthma
Sleep studies using polysomnography have suggested that people who have sleep disruption have elevated night-time levels of circulating cortisol and adrenocorticotropic hormone. They also have an elevated metabolic rate, which does not occur in people who do not have insomnia but whose sleep is intentionally disrupted during a sleep study. Studies of brain metabolism using positron emission tomography (PET) scans indicate that people with insomnia have higher metabolic rates by night and by day. The question remains whether these changes are the causes or consequences of long-term insomnia.
Mechanism
Two main models exists as to the mechanism of insomnia, cognitive and physiological. The cognitive model suggests rumination and hyperarousal contribute to preventing a person from falling asleep and might lead to an episode of insomnia.
The physiological model is based upon three major findings in people with insomnia; firstly, increased urinary cortisol and catecholamines have been found suggesting increased activity of the HPA axis and arousal; second, increased global cerebral glucose utilization during wakefulness and NREM sleep in people with insomnia; and lastly, increased full body metabolism and heart rate in those with insomnia. All these findings taken together suggest a deregulation of the arousal system, cognitive system, and HPA axis all contributing to insomnia. However, it is unknown if the hyperarousal is a result of, or cause of insomnia. Altered levels of the inhibitory neurotransmitter GABA have been found, but the results have been inconsistent, and the implications of altered levels of such a ubiquitous neurotransmitter are unknown. Studies on whether insomnia is driven by circadian control over sleep or a wake dependent process have shown inconsistent results, but some literature suggests a deregulation of the circadian rhythm based on core temperature. Increased beta activity and decreased delta wave activity has been observed on electroencephalograms; however, the implication of this is unknown.
Around half of post-menopausal women experience sleep disturbances, and generally sleep disturbance is about twice as common in women as men; this appears to be due in part, but not completely, to changes in hormone levels, especially in and post-menopause.
Types
Insomnia can be classified as transient, acute, or chronic.
- Transient insomnia lasts for less than a week. It can be caused by another disorder, by changes in the sleep environment, by the timing of sleep, severe depression, or by stress. Its consequences – sleepiness and impaired psychomotor performance – are similar to those of sleep deprivation.
- Acute insomnia is the inability to consistently sleep well for a period of less than a month. Insomnia is present when there is difficulty initiating or maintaining sleep or when the sleep that is obtained is non-refreshing or of poor quality. These problems occur despite adequate opportunity and circumstances for sleep and they must result in problems with daytime function. Acute insomnia is also known as short term insomnia or stress related insomnia.
- Chronic insomnia lasts for longer than a month. It can be caused by another disorder, or it can be a primary disorder. Common causes of chronic insomnia include persistent stress, trauma, work schedules, poor sleep habits, medications, and other mental health disorders. People with high levels of stress hormones or shifts in the levels of cytokines are more likely than others to have chronic insomnia. Its effects can vary according to its causes. They might include muscular weariness, hallucinations, and/or mental fatigue.
Prevention
Prevention and treatment of insomnia may require a combination of cognitive behavioral therapy, medications, and lifestyle changes.
Among lifestyle practices, going to sleep and waking up at the same time each day can create a steady pattern which may help to prevent insomnia. Avoidance of vigorous exercise and caffeinated drinks a few hours before going to sleep is recommended, while exercise earlier in the day may be beneficial. Other practices to improve sleep hygiene may include:
- Avoiding or limiting naps
- Treating pain at bedtime
- Avoiding large meals, beverages, alcohol, and nicotine before bedtime
- Finding soothing ways to relax into sleep, including use of white noise
- Making the bedroom suitable for sleep by keeping it dark, cool, and free of devices, such as clocks, cell phones, or televisions
- Maintain regular exercise
- Try relaxing activities before sleeping
Management
It is recommended to rule out medical and psychological causes before deciding on the treatment for insomnia. Cognitive behavioral therapy is generally the first line treatment once this has been done. It has been found to be effective for chronic insomnia. The beneficial effects, in contrast to those produced by medications, may last well beyond the stopping of therapy.
Medications have been used mainly to reduce symptoms in insomnia of short duration; their role in the management of chronic insomnia remains unclear. Several different types of medications may be used. Many doctors do not recommend relying on prescription sleeping pills for long-term use. It is also important to identify and treat other medical conditions that may be contributing to insomnia, such as depression, breathing problems, and chronic pain. As of 2022, many people with insomnia were reported as not receiving overall sufficient sleep or treatment for insomnia.
Sleep hygiene
Sleep hygiene is a common term for all of the behaviors which relate to the promotion of good sleep. They include habits which provide a good foundation for sleep and help to prevent insomnia. However, sleep hygiene alone may not be adequate to address chronic insomnia. Sleep hygiene recommendations are typically included as one component of cognitive behavioral therapy for insomnia (CBT-I). Recommendations include reducing caffeine, maximizing the regularity and efficiency of sleep episodes, minimizing medication usage and daytime napping, the promotion of regular exercise, and the facilitation of a positive sleep environment. The creation of a positive sleep environment may also be helpful in reducing the symptoms of insomnia. On the other hand, a systematic review by the AASM concluded that clinicians should not prescribe sleep hygiene for insomnia due to the evidence of absence of its efficacy and potential delaying of adequate treatment, recommending instead that effective therapies such as CBT-i should be preferred.
Epidemiology
Between 10% and 30% of adults have insomnia at any given point in time and up to half of people have insomnia in a given year, making it the most common sleep disorder. About 6% of people have insomnia that is not due to another problem and lasts for more than a month. People over the age of 65 are affected more often than younger people. Females are more often affected than males. Insomnia is 40% more common in women than in men.
There are higher rates of insomnia reported among university students compared to the general population.
Society and culture
The word insomnia is from Latin: in + somnus "without sleep" and -ia as a nominalizing suffix.
The popular press have published stories about people who supposedly never sleep, such as that of Thái Ngọc and Al Herpin. Horne writes "everybody sleeps and needs to do so", and generally this appears true. However, he also relates from contemporary accounts the case of Paul Kern, who was shot in wartime and then "never slept again" until his death in 1943. Kern appears to be a completely isolated, unique case.
See also
 In Spanish: Insomnio para niños
In Spanish: Insomnio para niños